Breast Health & Thermography
Non-invasive| Safe | Accurate | No Radiation | Painless | Non-contact | State-of-the-art Equipment
What is breast thermography?
It is a thermal measurement of breast surfaces for assessing breast health. To support early prevention of some breast problems. Infrared Breast Thermography is an imaging of the temperatures on the surface of the breast and can show some physiologic changes in the breasts that can help assess breast health changes. It does not replace Ultrasound, Mammography and/or MRI but according to the FDA is an adjunct to mammography. Thermography and Mammography are different, and both have an important role to play. Here is a comparison of the most important differences
Thermogram vs. Mammogram?
Thermography.
A non invasive, no radiation, no touch method of imaging the patterns of heat given off by your body. The associated patterns reflect different aspects of breast health.
Functional assessment: Thermal pattern changes are reflective of physiological or functional changes.
Preventive: Most useful before there is a cancer to assess breast health and physiologic changes and can help navigate in our efforts towards improved breast health.
Mammography.
Radiation and compression are used to produce a radiological image of the inside of the breast.
Structural assessment: The x-rays provide an image of a structure such as a mass, lump, or calcifications once they are large enough to be seen.
Corrective Treatment: To help detect a tumor after it is present. Once a tumor is detected, there is the possibility of biopsy, surgery, chemotherapy and /or radiation.
FAQs
Can thermography tell me if I have cancer?
Thermal breast imaging is a functional test to evaluate temperature as an indicator of physiological, metabolic and/or vascular (blood vessel) activity. Increased heat, which a thermogram may image, include a variety of conditions including cancer, inflammation, infection, healing scars, benign tumors and more. An abnormal thermal finding is not a guarantee that cancer is present, nor is a low T.H. rating of a thermal image a guarantee that cancer is not present. Thermal imaging is an adjunctive proceedure and does not replace other tests. It is not independently diagnostic of pathology. Thermography is a topographical infrared mapping technology, which does not see inside the body. When a thermogram shows an abnormal pattern, other imaging is necessary to evaluate for disease.
Will it tell me if I am helping or hurting my breast health?
Thermal pattern change can reflect breast health changes over time. Changes in diet, lifestyle, hormonal support etc. can change breast health and therefore the level of suspicion. This is reflected in a pattern change on the thermogram.
Can I do something about my breast health?
Yes! It is easy to increase your breast health with better lifestyle and dietary choices. Thus, the thermographic assessment can improve as the thermographic patterns improve. Breast thermography is most effective when used to monitor breast health over time. Each woman has unique thermal patterns which should remain stable over time, with only minor changes from year to year. Thus, a baseline image is important for initial evaluation while follow-up Thermograms help identify physiologic changes, which may warrant additional testing.
Who can benefit from Thermography and what is the process?
Women of all ages can benefit from thermography.
What distinguished thermography at Center for Health and Healing?
At CHH, we adhere to the American Academy of Thermology (AAT) guidelines for technique, assessment and resolution. These guidelines are internationally peer reviewed and they are the strictest, most comprehensive guidelines in thermography. The quality of the images is the highest at CHH and a full thermogram includes:
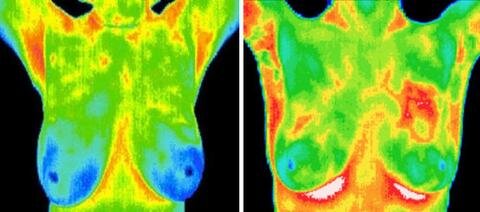
Color images for seeing regional heat patterns
Gray scale images for identifying certain thermovascular patterns associated with increased or decreased suspicion
A cold challenge with each full breast thermogram. The cold challenge consists of placing (gloved) hands in cold water to trigger a 'chill response'. Healthy areas tend to have a uniform and healthy cooling response. Tumors often don't cool or actually become warmer. This often makes the unhealthy area 'stick out' as having a different response than the healthy areas.
Ten views/images: our report typically includes 5 color and 5 gray scale views and may include additional views
Comparison for symmetry of various areas on each breast. Right/left symmetry is the most important criteria for assessing breast health. Suspect areas are outlined and their temperature precisely measured at thermal resolution of at least 0.1C) and are compared in order to assess level of suspicion. Specific temperatures over the breasts are measured, recorders and analyzed for significance.
Interpretation of each thermogram done by an AAT Certified Board Member (Bruce Rind, MD), adhering to the peer reviewed, internationally accepted guidelines. In addition to his AAT certification, he has been an integrative physician for over 45 years and has extensive experience in osteopathic mobilization. Working with the combination of thermography and osteopathic medical techniques has given Dr. Rind a unique perspective on relating structural health (e.g. rib cage dysfunction) to breast health. He has made presentations on this topic at the American Academy of Thermology.
Use of the internationally recognized (numerical) thermobiological (TH) rating system, in which the thermographic assessment ranges from normal of TH 1 to high index of suspicion of TH 5. The different thermobiological risk ratings are statistically associated with different risk levels
What to expect.
After the thermographic image has been analyzed, you will be given a copy for your records, as well as the option to discuss the results in detail with Dr. Rind or another physician knowledgeable in thermography. If the scan suggests that a thermogram ranges from normal to highly suspicious. You may decide to follow up with a consultation to determine next steps.
Next steps may include taking action towards improving breast health, as well as the possibility of pursuing other imaging services including: mammography, ultrasound, MRI or PET scan. Even though the thermographic image can be used for health assessment, an image suggestive of high suspicion could be an indicator of a problem coming on and closer monitoring might be warranted.
Is there a choice of scans?
The full scan consists of 9 thermal images followed by a cold challenge. Another 9 images are then taken. Both types of imaging allow a baseline image for monitoring future changes. In a cold challenge test, hands are placed in cold water for a minute. There is a reflex cooling of the body's skin in response to the cooling of the hands. Abnormal tissues tend to ignore the brain's orders to cool thus staying warm while the surrounding areas cool. A failed cold challenge is not proof of malignancy but raises our level of suspicion.
$275
Full Breast Scan
Fee includes a written assessment/report with the thermographic images. It does not include review with the practitioner. Since thermography is preventive medical care, it is not likely to be reimbursed by insurance.
*Referenced articles
-Parisky, Y R, et al. Efficacy of Computerized Infrared Imaging Analysis to Evaluate Mammographically Suspicious Lesions. American Journal of Roentgenology, January 2003, 263-69. The article states that Th-1 and Th-2 (i.e., thermographic risk levels 1 and 2) scores can be reassured with a 99% level of confidence that they do not have breast cancer.
-The Breast Journal, Volume 4, 1998, 245-51, Keyserlingk et al documented 85% sensitivity in diagnosing breast cancer using clinical examination and mammography together. This increased to 98% when breast thermography was added.
-Gautherie, M, and Gros, C M. Breast Thermography and Cancer Risk Prediction. Cancer, 1980, volume 56, 45-51: The article reports that fiftyeight thousand patients with breast complaints were examined between 1965 and 1977. 1,245 patients with abnormal Th-3 mammotherms had normal breasts by mammography, ultrasound, physical exam, and biopsy. 38% percent of women with normal breasts and 44% of those with mastopathy (i.e., breast problem) developed biopsy proven breast cancer within five years. In 90% of patients with a Th-4 or Th-5 (thermographic risk level of 4 or 5), a diagnosis of cancer was made on their first visit.